How to prevent falls?
In Norway, approximately 9,000 adults suffer from hip fractures each year. Read how Dr. Remi Andersen from Ullernhjemmet Nursing Home in Oslo believes that a tool like Somnofy can contribute to preventing falls!
As a child, you fell repeatedly - yes, the foundation for learning to walk was to try, fall, and get up again. The goal was to find the delicate balance where the body was in equilibrium and when it wasn't. Because the question is - can one be in balance while walking? The answer is actually no. When you walk, the body is in a state of falling - and what prevents you from falling to the ground is the body's ability to correct this by moving the legs forward. If not - well, then you stand still.
The same repeated itself when you were learning to skate or ski; Falling to move forward, bumps and falls before mastering the technique - and up again.
The point is: One must practice mastering gravity. What you practice is what you become good at!

Falls in the Elderly
Much is written about falls among the elderly. The truth is that most of us experience a fall at some point during the year. However, the consequences become much greater as one gets older - primarily due to a reduction in bone mass with age, making it less resilient to the same strain.
Falls among the elderly result in significant personal suffering and incur substantial costs for society. The report 'Costs of Hip Fractures in the Elderly' (1) from 2014, based on a sample of home-dwelling individuals over 70 years in Sør-Trøndelag, estimated the average cost at NOK 322,000 per hip fracture incident. If the fall led to a permanent nursing home placement, the annual cost rose to a staggering NOK 953,000.
The Risk of Hip Fractures Increases with Age
In Norway, approximately 9,000 adults suffer from hip fractures each year. In other words, a hip fracture occurs every hour. Seven out of ten hip fractures affect women and the risk of fractures sharply rises from the age of 70.
Small Changes - Significant Impact
The risk of falls can be assessed using various scoring tools. Generally, emphasis is placed on previous falls, reduced vision, dementia/confusion, agitation/wandering tendencies, frequent bathroom visits, ability to move between bed and chair, walking function, use of multiple medications in general, and tranquilizers or sleep medications in particular.
As mentioned earlier, mastery comes from consistent practice.
Falls in nursing homes often occur during the transition from lying down to standing or when using the bathroom in the resident's own room at night. Throughout a day, there are limited instances when the resident is in such a situation. However, if the healthcare workers actively encourages the patient to stand up and sit down 5 times instead of 1 when getting out of bed or a chair, with minimal effort, they effectively train 400% more in a day. As mentioned, proficiency comes from consistent practice.
Når det gjelder risiko i omgivelsene er det viktig å legge til rette for godt lys, sklisikre underlag, fravær av terskler/kanter/løse tepper samt godt skotøy.
Falls Create Insecurity and Reduced Quality of Life
Elderly individuals who have experienced a fall are often afraid of falling again. This quickly leads to a vicious cycle of reduced activity, isolation, loss of independence, and increased dependence on care. Therefore, fall prevention is crucial.
Can Welfare Technology Contribute to Fewer Falls?
Dementia is a widespread diagnosis both in nursing homes and among the elderly who require home care services. A significant challenge is that this group struggles to absorb information – and, most importantly, remember it – regarding fall prevention measures. Walkers are often left behind when residents go to the bathroom or into the living room. They forget that they are unsteady and neglect to seek help through devices such as pull cords or room alarms.
Many people with dementia may also reverse their sleep patterns and leave their beds at night. It is challenging for limited night staff to detect this before it's too late, and the resident has fallen.
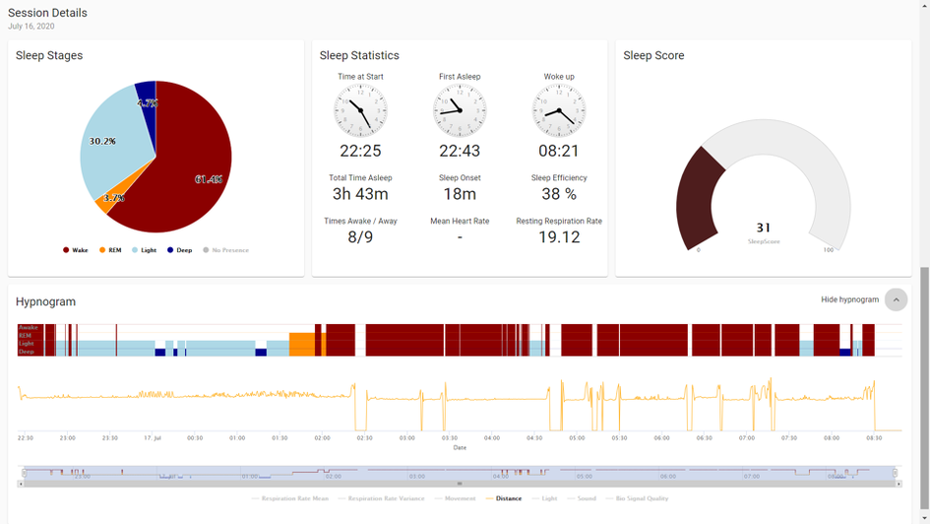
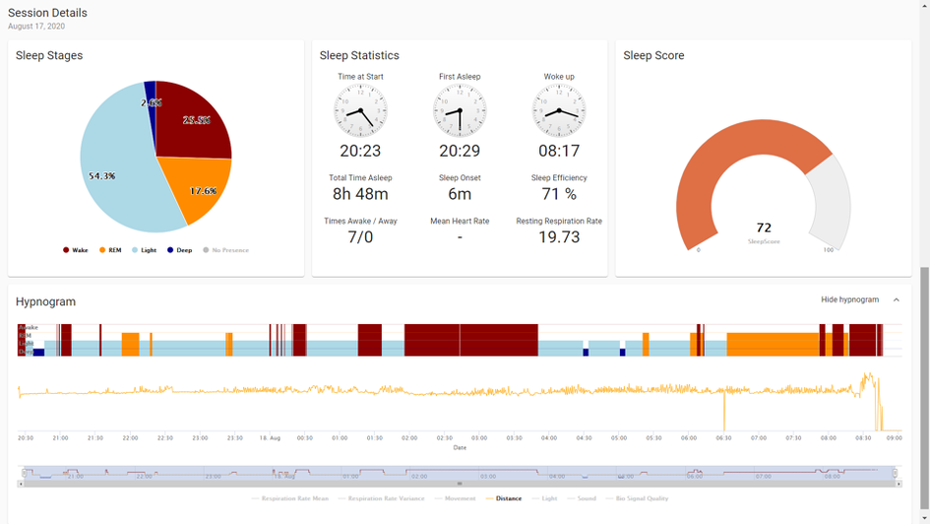
Through the monitoring of sleep patterns in selected individuals in the nursing home, we have observed, using our tool Somnofy, how some residents get up 6-10 times during the night, without the staff being aware of it. Such monitoring has been crucial for understanding the risk of falls in individual rooms and the opportunity to take measures to reduce nighttime wandering.